That is according to an article in JAMA based on a report from the Center for Healthcare Quality and Payment Reform. The report states:
More than half (55%) of the rural hospitals in the U.S. do not offer labor and delivery services, and in 10 states, more than two-thirds do not. Over the past decade, more than 200 rural hospitals across the country have stopped delivering babies…
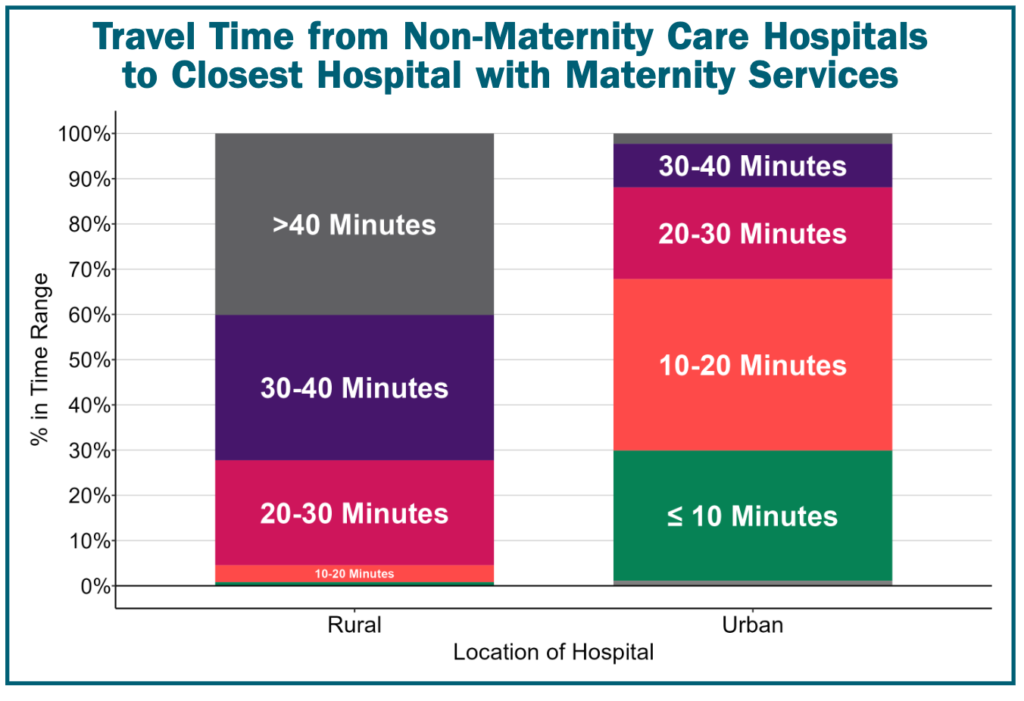
In most urban areas, the travel time to a hospital with labor and delivery services is under 20 minutes, but in rural areas, the travel time is likely to be at least 30 minutes, and it is often 40 minutes or more.
https://ruralhospitals.chqpr.org/downloads/Rural_Maternity_Care_Crisis.pdf
The longer travel distances impact not only access to care during delivery, but also prenatal and post-natal care.
The absence of local maternity care services is felt throughout the continuum of obstetric care. Patients are less likely to obtain adequate prenatal or postpartum care services if they need to travel long distances.
“It’s one thing to say the mother has to drive half an hour to deliver her baby,” Miller said. “It’s another thing to say the mother has to drive a half an hour every month to be able to get prenatal care. They can’t take time off of work, can’t take time away from the kids.”
https://jamanetwork.com/journals/jama/fullarticle/2815499
Why are rural hospitals dropping maternity care? Clearly the answer is that reimbursement is far below their cost. Moreover, finding adequate staffing is difficult.
Maintaining labor and delivery services requires having physicians and nurses, including nurse anesthetists or anesthesiologists, who are trained and available around the clock to manage deliveries as needed. As a result, payments per birth that are adequate at a large hospital are not enough to support maternity care at small rural hospitals with far fewer births.“We deliver about 300 babies a year, so an average of less than 1 a day, but you still have to have OB-GYN coverage 365 days a year, 24 hours a day, 7 days a week because babies come at all times,” Sinek said in an interview. “It’s costing us $7.5 million right now to staff our OB unit with nurses that know what they’re doing and CRNAs [certified registered nurse anesthetists] to do anesthesia services and the office staff to support that care. All of that is really adding up, and if you don’t deliver enough babies to cover those costs, then you’re on a downhill course.”
…fewer obstetricians and family physicians with obstetric skills are able or willing to be on call several nights and weekends out of every month…As a result, hospitals either must employ or contract with more physicians or OB-GYN hospitalists.
https://jamanetwork.com/journals/jama/fullarticle/2815499
You can read the full report here.


















